Sterilization is the process of eliminating all microorganisms from a particular site to reduce the transmission of diseases associated with the use of the said site. Sterilization aims to create an infection-free hospital environment, especially because health centers receive a large number of patients with disabilities and various illnesses. Infection control ensures the success of the surgery, as surgical interventions make patients vulnerable to germs if they are not completely sterile because medical instruments that come into contact with body tissues or fluids are considered critical elements that must be sterilized when used to reduce organism transmission to the patient.
Therefore, the CSSD is one of the most important pillars of the hospital. The Central Sterile Services Department at Imam Al-Hujjah Hospital is unmatched in the history of this country. It was designed and equipped by the Italian company of infection control “CISA”. The contaminated materials and equipment have their own entrance and exit that are completely separate from the sterile materials and equipment route.

This area is the first stop for the receipt of contaminated surgical materials, devices, and kits which are carried from the operating theater by portable, locked trolleys. Technicians wash these materials by sonication to dissolve the remnants of tissues and clotted waste from the surgical tools and devices.
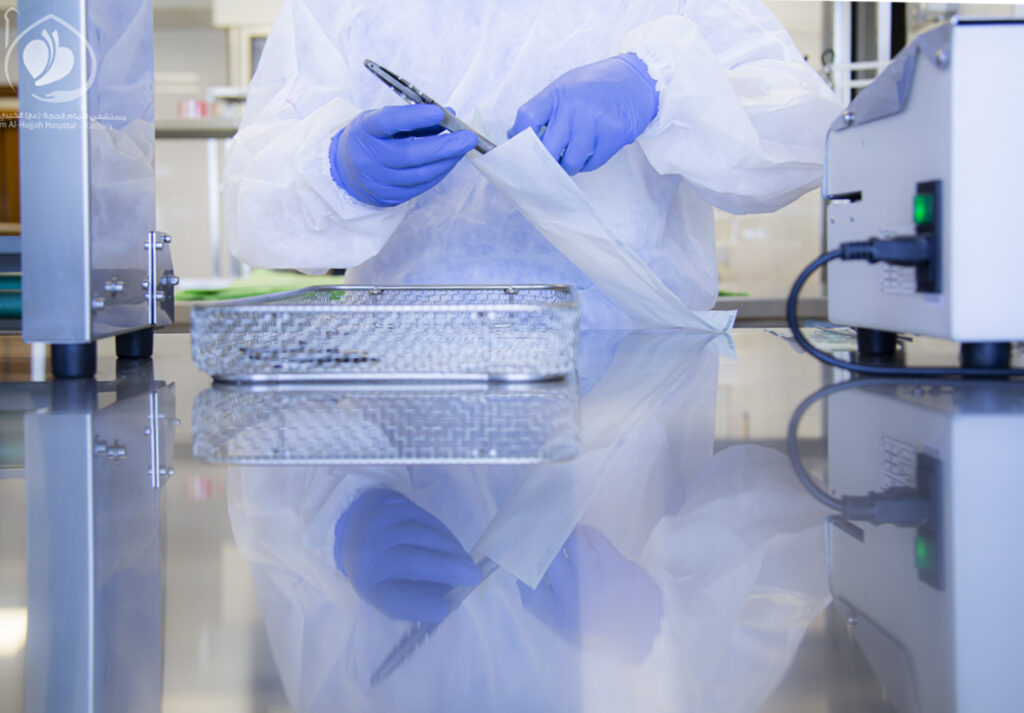
This area is completely separate from the “Dirty Zone”. Surgical instruments are sent to anti-contamination washers/disinfectors that dissolve viruses and proteins from surgical items. Technicians examine those instruments using electron microscopes to ensure that they’re completely free from residue. Then the technicians pack the equipment and place them in thermal and non-thermal sterilizers.
After thermal and non-thermal sterilization, surgical kits and devices are sent to this area for storage. Most surgical instruments are made of heat-resistant materials, therefore they can be subjected to high temperature during steam sterilization. Certain surgical instruments are made of materials that are not heat-resistant, requiring low-temperature sterilization. In the new sterilization systems with low temperatures, such as plasma and hydrogen peroxide gas sterilization, both thermal and non-thermal sterilizers are used. Then the materials are stored in this ultra-clean zone.
The sterile medical equipment and supplies are transported in a double-door container from the third zone to the operating theater via a special elevator after passing through the delivery zone.
This sterilization process prevents mixing contaminated and sterile instruments, thus reducing contamination levels in operating theaters and ultimately providing a safe environment for the patient that protects him from complications and health problems.


The goal of implementing the infection control program is to prevent or stop the spread of contagious diseases among patients and employees in healthcare facilities. This can be accomplished through a set of policies, guidelines, and preventive measures. Standard procedures are used on the basis of risk assessment, and personal protection methods are implemented to protect healthcare providers and prevent the spread of infection from patient to patient, in addition to applying all methods and means to provide a clean environment free of any infection, especially in the operating rooms.



1) Following the guidelines set by international authorities, such as the World Health Organization and the Joint Commission International, in addition to locally approved sources (the National Guidelines of Infection Control).
2) Education and training in accordance with the “Best Practices in Healthcare”.
3) Monitoring the adoption and improvement of correct medical practices.
4) Monitoring, verifying, and following up on feedback to ensure whether the right thing is happening at the right time. Continuous improvement, performance evaluation, data collection, and comparing performance before and after the change.
5) Establishing and creating a clean, pest-free environment, spaces, devices, and medical equipment by using internationally approved materials to sterilize medical devices and instruments.
6) Ensuring the safety of employees and providing a work environment free of infection through periodic checks, and providing sick leave for infected workers to prevent the spread, and reporting cases of needlestick injuries during work.
7) Preparing periodic reports and collecting samples for laboratory testing every month.
Imam Al-Hujjah Hospital attaches great importance to supporting the infection control program by providing the latest technology, supplies, and special means that help prevent the spread of infection. Sterilization stations and washbasins were distributed in all hospital corridors and departments, in addition to informational and educational posters. One of the most important and simplest rules for infection control is handwashing and using hand sanitizers.
Imam Al-Hujjah Hospital pays constant attention to providing a safe, contamination-free environment. We believe that the most important pillar of work is to maintain the safety of the patient and his escort, as well as the safety of employees.



This is a hospital-acquired infection, and symptoms may not appear until after 72 hours or more. It’s also called “Nosocomial Infection”.
The infection control unit at Imam Al-Hujjah Hospital, is an important part of the healthcare infrastructure. It strives to provide all protection arrangements in order to prevent hospital-acquired infection. Such arrangements include:
1. Preparing all qualified staff (medical, nursing, healthcare, engineering, technical, administrative, and cleaning workers) who are trained to provide services in accordance with quality standards and full adherence to the international principles of infection control.
2. Continuous follow-up and regulation of infection control procedures, correcting them if necessary, and improving them continuously.
3. Providing valid and effective materials and supplies (for sterilization, disinfection, and fumigation) and evaluating them by modern scientific methods.
4. Monitoring and control by collecting monthly contamination swabs, technical checklists, and recording any breach.
5. Periodic evaluation and support of studies and research to develop the performance of infection control programs.
The program consists of the following procedures:
First) Cleaning: The hospital follows a daily cleaning program consisting of:
1. General cleaning: Thorough daily cleaning tours of all rooms and corridors.
2. Personal Hygiene: It includes all hospital workers:
a- Handwashing:
• Routine washing.
• Hygienic handwashing (for healthcare providers).
• Surgical handwashing (for medical and nursing staff).
b- Showering (for employees and patients).
Second) Disinfection and Sterilization, using the following methods:
1. Autoclave.
2. Active and inert chemicals, solutions, and gases.
3. Ultraviolet radiation.
4. Nanofiltration.
Third) Separating and collecting waste. Safe and proper disposal of waste (via burning, shredding, burying, or recycling).
Fourth) Providing personal protective equipment for all employees, patients, and visitors of the hospital.
5) Activating the role of the infection control unit in cooperation with all departments.


جميع الحقوق محفوظة لمستشفى الامام الحجة (عج) الخيري © 2023